Improve your quality of life with cataract surgery or lens replacement.
What is a cataract?
A cataract is a clouding or opacity of the natural lens inside our eye. The lens sits in the eye, behind the coloured part of the eye (the iris). When cataract develops, the lens prevents light rays passing through or alters the pathway of these rays, resulting in objects not focusing sharply on the retina. This degrades the quality of vision.
Throughout life our lens gradually loses its natural elasticity, until the 5th decade of life when its ability to accommodate and focus for near objects becomes significantly compromised. This is known as dysfunctional lens syndrome or presbyopia. Over the next few decades the lens acquires a brownish hue; when the lens has lost its normal clarity and transparency, it is called a cataract.
What symptoms does cataract cause?
Cataracts are usually slow to develop over years, causing a gradual reduction and blurring of vision, a reduction in the sharpness or a degradation in the overall quality of vision. Glare may be noticed at night, even with early cataract; this may cause difficulty with night-time driving. Other symptoms may cause include double vision in one eye and the need for frequent change in spectacles.
A cataract does not cause pain or redness of the eye. However, if you are struggling to see clearly because of cataract and overusing your facial muscles in response, you may develop some headache over prolonged periods of detailed work.
How can a cataract be treated?
The only treatment for cataract is surgery. However, you do not need to have surgery if your eyesight is not affected.
During the operation, a small device is used to break up the lens and remove your cataract. A new clear lens, called intraocular lens (IOL), is then placed in the position of your old lens; it remains in the eye for the rest of your life. The IOL is made of plastic materials or derivatives, such as PMMA and silicone.
Cataract surgery can dramatically improve your quality of vision and life.
What benefits can I expect after cataract surgery?
-
Around 99% of patients have a significant improvement in vision following cataract surgery helping with driving, reading, working, hobbies, safety and self-confidence.
-
Cataract surgery provides the opportunity to correct pre-existing and underlying refractive errors, such as astigmatism, short-sightedness and long-sightedness.
-
In addition, cataract surgery provides a great opportunity to reduce or eliminate the need for reading glasses.
-
Co-existing eye conditions, such as macular degeneration or glaucoma, can limit the extent of improvement after surgery. However, if a significant cataract is present, cataract extraction surgery can provide a substantial improvement in the quality of your vision and life.
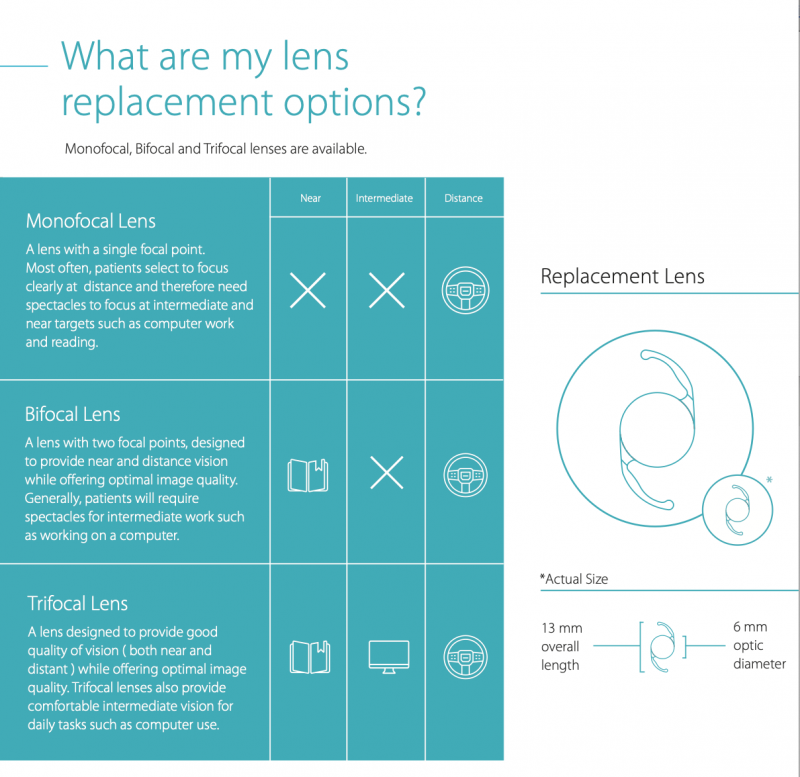
What are my new lens options for cataract surgery?
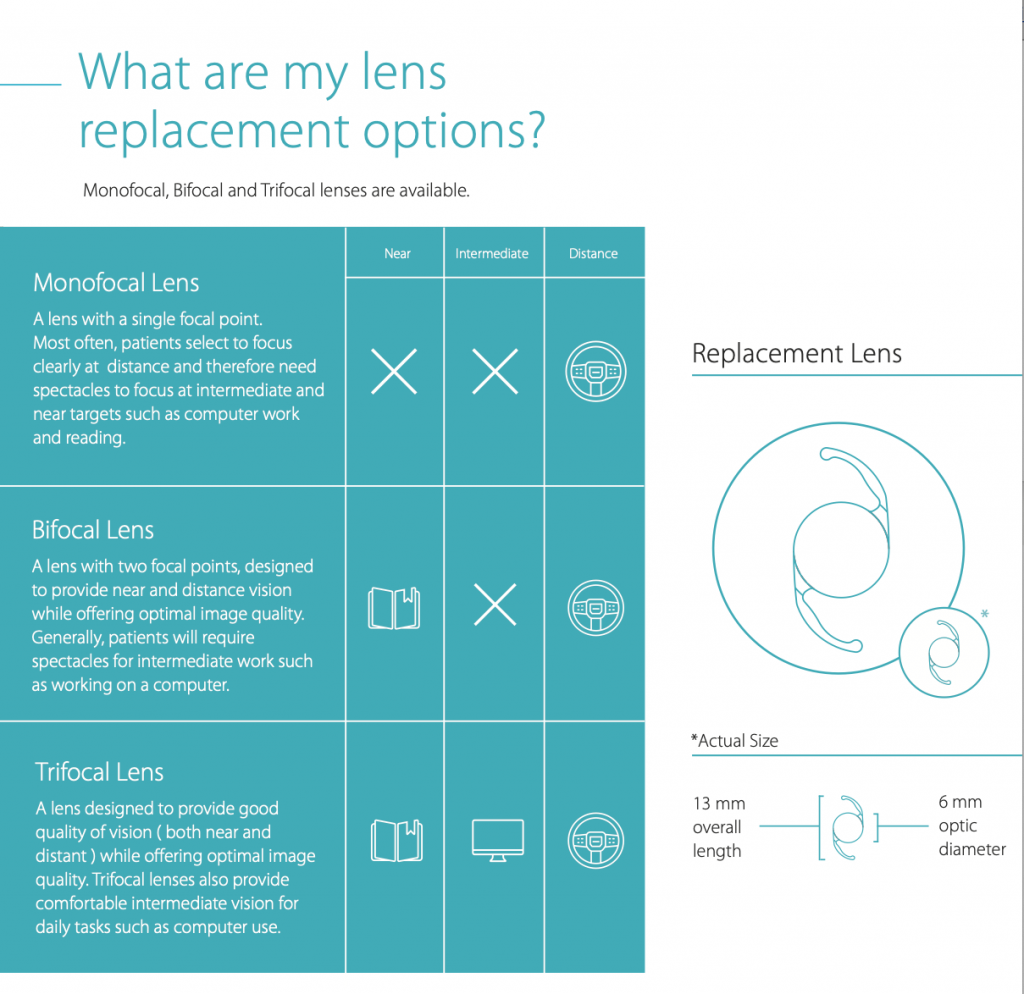
Monofocal lens
This is the standard lens used for the majority of cataract operations in the UK, including the NHS. It provides good quality vision but it cannot provide clear vision for both distance and near; reading glasses will be needed for all near activities.
A monofocal lens can be combined with astigmatism reduction. This allows us to achieve the best possible distance vision without glasses. Reading glasses will be needed.
Reading and near vision can however be achieved with the use of monofocal lens:
-
Monovision focuses one eye for distance and the other eye for near, with appropriate selection of monofocal lens. A refractive work-up is carried out to assess your suitability and tolerance of monovision.
-
PRESBYOND laser blended vision is a laser vision correction procedure that can be carried out after standard cataract surgery with a monofocal lens. The principle is similar to monovision (one eye focused for distance, the other for near) but there is a smoother transition between the two eyes. A refractive work-up is carried out to assess your suitability and tolerance for this procedure.
Multifocal lens
A trifocal lens provides overall good quality vision, achieving clear vision for both distance and near without glasses. The visual performance of this lens favours distance and near vision. The vast majority of patients can read very small print, however a weak pair of glasses may be needed for prolonged computer use.
This lens can be combined with astigmatism reduction, allowing us to achieve the best possible vision without glasses. A refractive work-up is carried out to assess your suitability.
Extended depth of focus lens
An extended depth of focus lens provides good quality vision, achieving clear vision for both distance and near without glasses. As the visual performance of this lens favours distance and intermediate vision, a weak pair of reading glasses may be needed for reading small print, especially in dim light.
This lens can be combined with astigmatism reduction, allowing us to achieve the best possible vision without glasses. A refractive work-up is carried out to assess your suitability.
Cataract Surgery FAQs
From the early years of our life there is natural decline in the elasticity of the normal lens inside your eye. This results in the lens losing its ability to accommodate and therefore focus at a range of distances. Once this causes difficulty or sluggishness in focusing for near objects, the condition is called dysfunctional lens syndrome or presbyopia.
Similar lens changes continue throughout life. Later on in life the lens assumes an increasingly brown hue and loses its transparency over many years and decades. The lens is described as a cataract when it has lost this transparency.
Other common causes for development of cataract, especially at a younger age, include metabolic disorders, such as diabetes, chronic corticosteroid use, trauma to the eye and previous eye surgery. Smoking and chronic exposure to sunlight have also been described as risk factors.
The presence of a cataract can be diagnosed by your optometrist or ophthalmologist (eye doctor).
At this clinic visit your eyes will be examined with specialist equipment that magnify the view into your eyes. Your pupils are normally dilated (enlarged) at this assessment; as this will blur your eyesight for a few hours it is important that you do not drive.
A cataract assessment provides a good opportunity to exclude other conditions that may also be contributing to a reduction in quality of vision, such as dry eye, glaucoma and age-related macular degeneration. Their presence doesn’t preclude successful cataract surgery.
You can continue to drive if you have a cataract, provided you meet the standards of vision for driving and do not experience visually significant glare. However, if you have been diagnosed with cataract, surgery to remove your cataract will almost certainly improve the quality of your vision.
In order to drive in the UK you must be able to read (with glasses or contact lenses, if required) a car number plate made after 1 September 2001 from 20 metres. You must also meet the minimum eyesight standard for driving by having a visual acuity of at least decimal 0.5 (6/12) measured on the Snellen scale using both eyes together. This will be assessed at your clinic consultation.
There is a common historical misconception that your cataract needs to be ‘ripe’ or ‘mature’ in order to have surgery. This could not be more incorrect. Once a cataract that degrades the quality of your vision has developed, surgery can be safely performed; indeed, it has been shown that advanced cataracts have a higher rate of complications during surgery.
Cataract surgery is a very safe procedure. It is the most frequently performed procedure in the UK, with more than 400000 surgeries performed annually. As with all operations, problems can develop during the operation or afterwards in the healing period. The National Ophthalmology Database Audit reported that less than 1 in 100 patients experienced visual loss after cataract surgery. The risk of serious loss of vision (vision worse than driving standards) is even smaller.
- In broad terms, IOL types and options include monofocal, multifocal and toric lenses.
- All patients undergoing cataract surgery have a lens (IOL) that is matched to their eye. The calculation of the power of this IOL is based on the eye measurements that are taken during your clinic visit. The power of the IOL will determine whether your natural vision (without glasses) is focused for distance, near or intermediate.
- Most patients prefer to have good distance vision without spectacles and the IOL power is selected accordingly. Spectacles however may still be needed following surgery for your best distance vision; this reflects technology limitations in predicting the IOL power that your eye may need.
- Laser refractive surgery after cataract surgery may be considered as a top-up treatment to provide you with the best distance vision without spectacles.
- All patients with a standard monofocal IOL will need spectacles for near vision, e.g. for reading.
- Monovision can be used with monofocal lenses; this focuses your dominant eye for distance and your other eye for near, reducing your need for spectacles for near activities.
Astigmatism is a common condition that causes blurred vision. It is usually caused by the presence of a non-uniform shape of the cornea or the development of abnormalities in the natural lens of your eye, such as cataract. Normally, the combined refractive efforts of the cornea and your natural lens focus light rays sharply on the retina of the eye. In astigmatism, the imperfect refractive properties of the eye result in an object not being uniformly focused on your retina and thus blurred vision. Cataract surgery provides a unique opportunity to address corneal astigmatism with the use of a toric lens (IOL); this will provide greater quality of vision and reduce dependency on glasses.
Very often the cornea is not a perfect sphere in shape, resulting in astigmatism; a toric IOL can be used with cataract surgery to compensate for this astigmatism. A toric lens greatly reduces or eliminates the need for spectacles after surgery, whether a monofocal or multifocal IOL has been used, and provides better quality vision. Detailed topography scans of the cornea are required to assess your suitability for a toric IOL.
A multifocal lens is a great option if you are interested in being less dependent on spectacles following surgery. It can provide clear vision for both distance and near without glasses. The majority of patients can read small print following surgery, however a weak pair of glasses may be needed for prolonged reading or computer use. This lens can also be combined with astigmatism reduction by using a toric multifocal lens; this would allow you to achieve the best possible vision.
As with all operations, problems can develop during cataract surgery or afterwards in the healing period. The National Ophthalmology Database Audit reported that less than 1 in 100 patients experienced visual loss after cataract surgery.
Complications during and after cataract surgery are uncommon, and most can be corrected with a second procedure. The most common complication during surgery is called posterior capsule rupture, a breakage in the posterior membrane of the natural lens. This occurs in approximately 1 in 100 patients and an additional step (anterior vitrectomy) may be required during surgery. Occasionally, in less than 1 in 200 patients, further surgery on another day may be required.
In the healing period, patients can occasionally develop clinically significant retinal swelling, cystoid macular oedema (approximately 1 in 100 patients); this can be treated with drops and sometimes a steroid injection. Less frequent complications, such as infection (less than 1 in 1000 patients), retinal detachment (less than 1 in 1000 patients), corneal decompensation, eyelid drooping can also develop.
The vast majority of patients require local anaesthesia for cataract surgery. Local anaesthesia is applied either as eye drops or an injection around the eye. Once you have been given a local anaesthetic you will still be awake and aware of what is happening, but you will feel no pain during the operation. Rarely, a general anaesthetic may be needed.
Local anaesthesia works very well at stopping you feel pain during the surgery and also offers pain relief after the operation. Generally, it has fewer risks and side effects than a general anaesthetic. You will recover more quickly and can go home on the same day. With local anaesthesia you can continue to take your usual prescribed medication and can eat and drink as normal after the operation.
When the operation starts you will see a bright light from the operating microscope. It is not unusual to see shadows, movements, or kaleidoscope effect lights during the operation, but you will not be able to see details of the operation. It is important that you look straight into this light and not move your eye by looking around. You will be aware that the surgeon is working and may feel pressure at times.
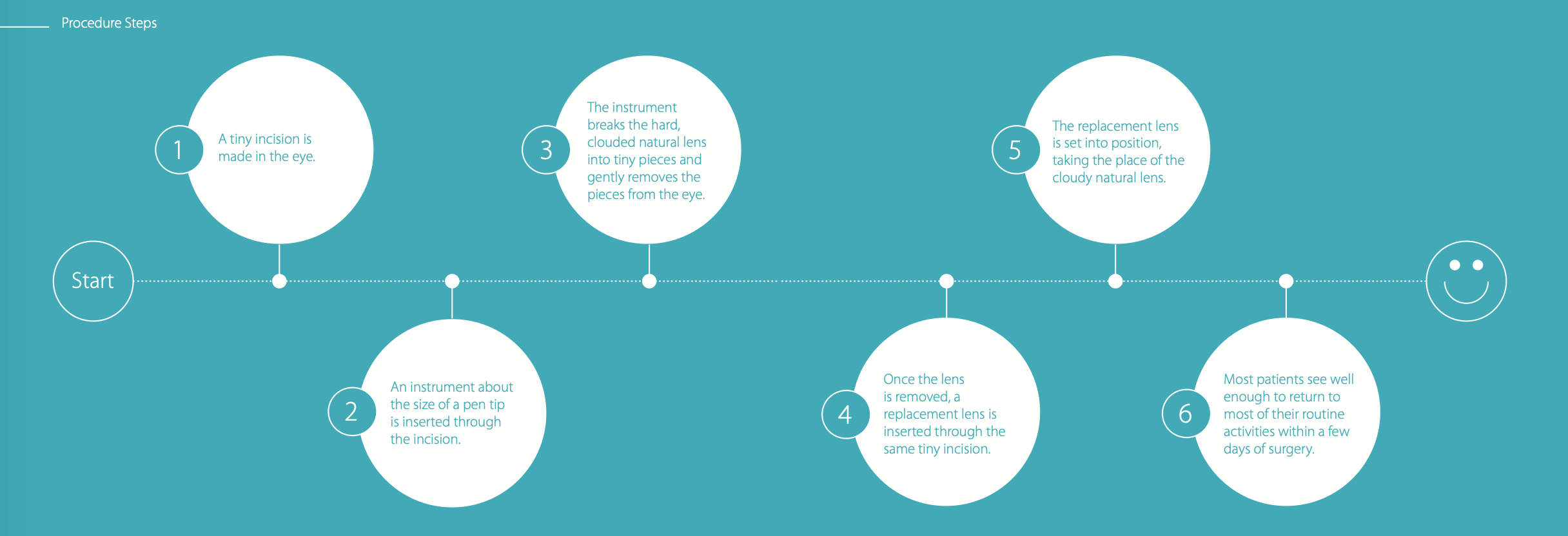
Cataract surgery is a simple and safe procedure requiring 15 to 30 minutes. A simplified explanation of the procedure can be provided by the following sequence of steps:
- Anaesthetic and antiseptic drops are applied.
- A tiny incision is made in the eye.
- An instrument about the size of a pen tip is inserted through the incision.
- The instrument breaks the hard, clouded natural lens (cataract) into tiny pieces and gently removes the pieces from the eye.
- Once the cataract lens is removed, a replacement lens (called the IOL) is inserted through the same tiny incision.
- The replacement lens (IOL) is set into position, taking the place of the cataract lens.
- No sutures are usually required.
Cataract surgery is not painful. A pressure feeling may be experienced at times during the surgery, but not pain. You may notice shadows, movements, or kaleidoscope effect lights during the cataract operation, but you will not be able to see detail. A slight gritty sensation and sensitivity to light may be noticed for the first 24-48 hours after the surgery, particularly as your pupil size may take a day or two to return to normal (the pupil is dilated for the purposes of surgery).
Once you have recovered from surgery, you may go home. You will have instructions about post-operative care and will be told about the medication you need to take. You will be shown how to put your eye drops in, if you are unsure what to do. Drops are used following surgery to reduce inflammation and to prevent infection.
Following surgery, the eye is generally comfortable, though a little scratchy. Your vision will be blurred for the first 24-48 hours, due to the surgery and a large pupil. It should then start to improve over the next few days. You may notice that the eye is slightly sensitive to bright light. Wearing dark glasses may help with this sensitivity and glare.
You may be able to drive within 3 to 4 days of surgery. Following surgery, you are legal to drive as soon as you can see a number plate at 20 metres. However, at the same time your eye must not be sensitive to light or uncomfortable.
You will be required to use drops following the surgery, typically for a month. Do take the drops that you have been provided with and stay in a clean, dust-free environment for at least 1 week. Also wear a protective shield at night for the first week; this will stop you rubbing or touching the eye when asleep.
Do not get the eye wet for 1 week; a bath instead of a shower and assistance with washing your hair may be advisable. A visit to the hairdresser’s may also be an option. I generally advise not to wear make-up for 2 weeks and not to lift heavy weights or do strenuous exercise for 2 weeks. Swimming and the use of a sauna should be avoided for one month.
Typically, this is within 3 to 4 days of surgery. Following surgery, you are legal to drive as soon as you can see a number plate at 20 metres. However, at the same time your eye must not be sensitive to light or uncomfortable in any way. Your vision will be blurred for the first 24-48 hours, due to the surgery and a large pupil. It should then start to improve over the next few days. You may notice that the eye is slightly sensitive to bright light. Wearing dark glasses may help with this sensitivity and glare.
Testimonial of patient happy with PanOptix multifocal lens