What is refractive lens replacement?
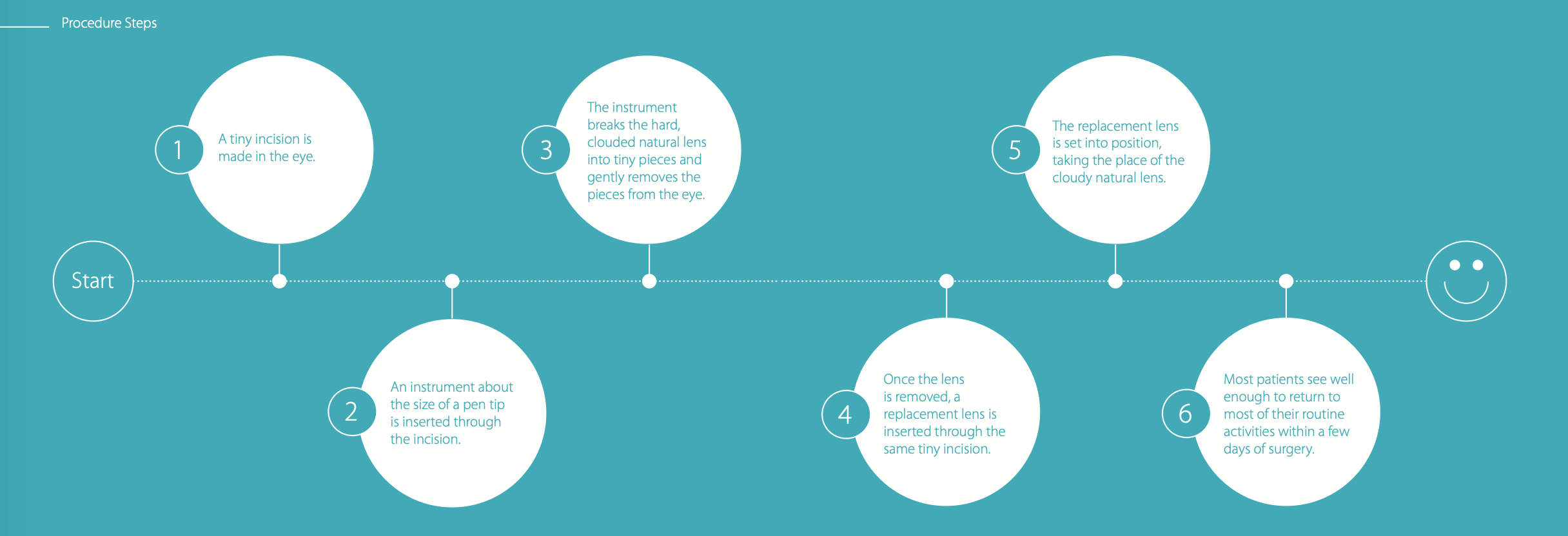
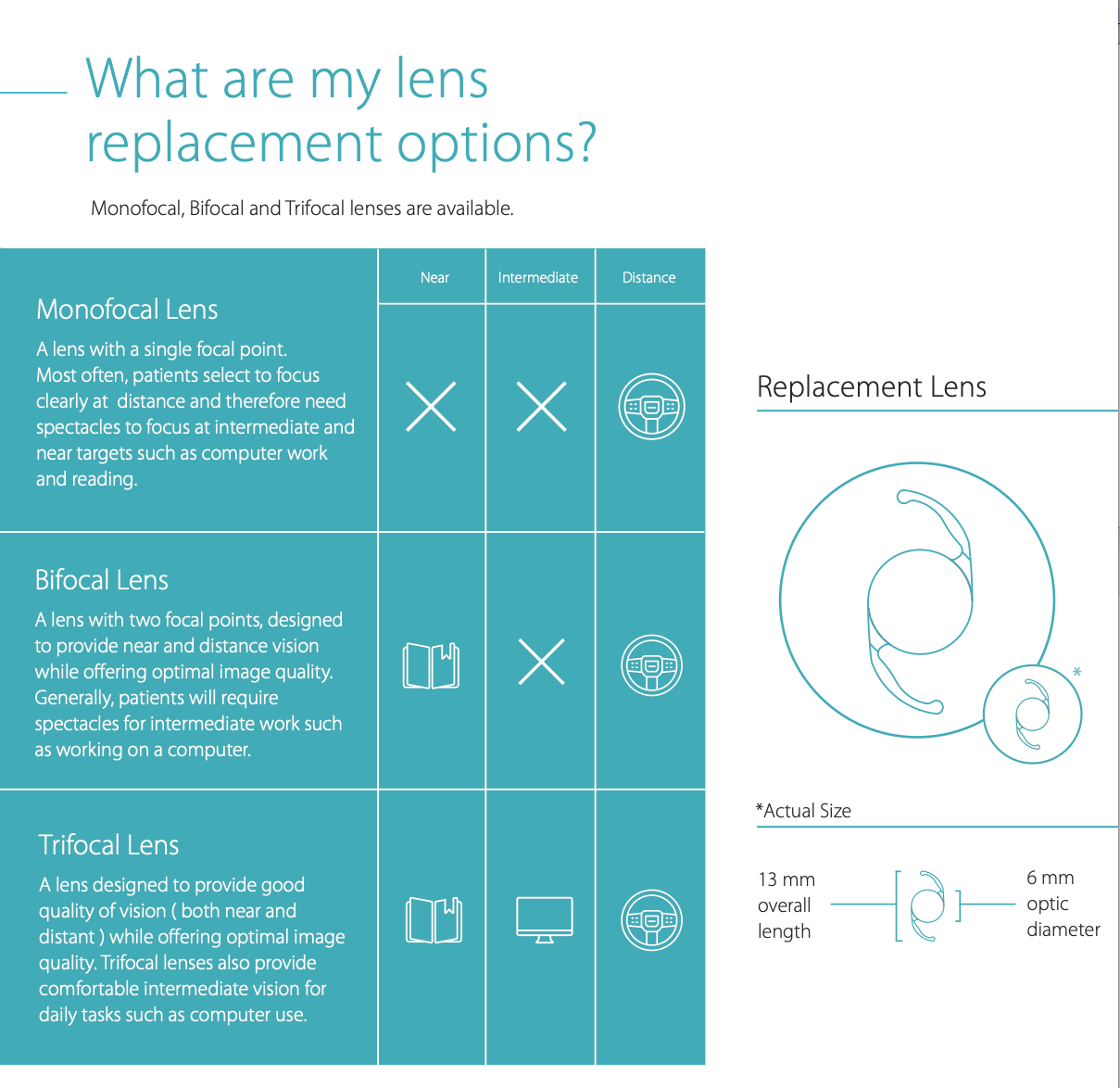
Refractive lens replacement, also known as refractive lens exchange, is very similar if not identical to modern cataract surgery. It involves replacing your natural lens with a new artificial intraocular lens, usually a special multifocal or extended depth of focus lens, that lasts for life. The lens sits inside the eye behind the iris, the coloured structure of the eye that gives us our green or brown eyes, and is normally clear and transparent.
As we get older the lens loses its natural elasticity and ability to focus, a condition called presbyopia or dysfunctional lens syndrome. Later in life, the lens loses its normal transparency and optical properties; at this stage it is called a cataract.
Refractive lens replacement can achieve freedom from glasses. In addition to addressing presbyopia (the need for reading glasses), it can also achieve clear distance vision without glasses by correcting underlying refractive errors of the eye, such as short-sightedness, long-sightedness and astigmatism.
Laser eye surgery can achieve similar results and may be the preferred procedure, especially under the age of 55 years.